A 33-year-old male long jump parasport athlete with a transtibial amputated leg suffered an ACL rupture from knee hyperextension, presenting a positive Lachman test and no frontal plane laxity. This case aims to discuss therapeutic options for ACL reconstruction, patient positioning, and graft choice.
- 33 Y.O male
- Long jump professional parasport
- ACL rupture on a transtibial amputated leg
- Mechanism: Knee hyperextension
- On physical examination, he presents a positive Lachman test and a negative pivot shift test, no laxity in the frontal plane at 0 and 30 degrees of flexion
The ACL Rupture
Imagery MRI
How would you treat the patient?
- ✔️ACL reconstruction with quadricipital tendon
Graft justification
Our patient is a professional in long jump, a discipline where sprinting is essential. Here, a hamstring graft is not relevant because the hamstrings provide propulsion in the absence of the triceps surae in an amputee patient. It therefore seemed unthinkable to reduce its propulsion capacities.
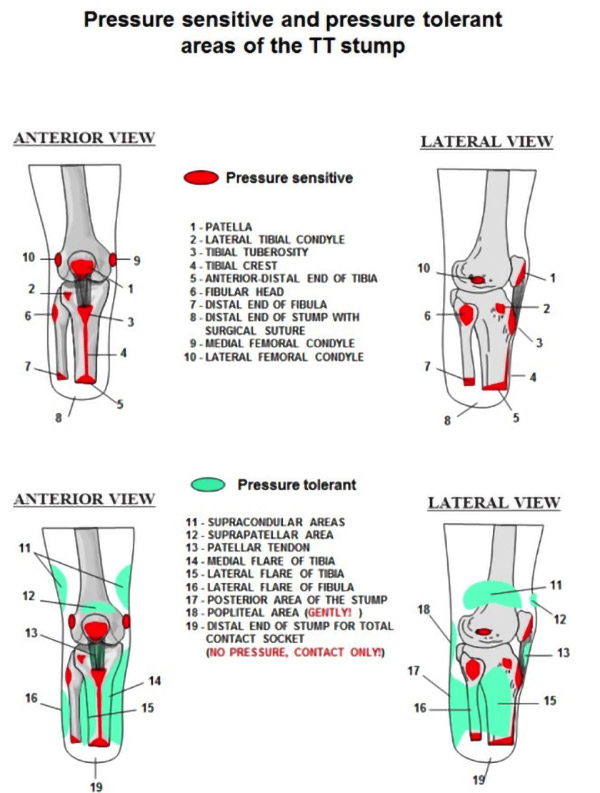
The tibial prosthesis is made up of a socket, a sleeve, a leg segment and a foot. The tibial socket must respect a distribution of support to obtain comfort and dynamism. The residual muscles of the stump exhibit contractions necessary to maintain the socket. It is therefore essential to understand the risks of friction and pressure on potentially sensitive areas.
The amputee patient presents a new muscular state, impacting on walking which becomes asymmetrical and more demanding in energy, the modified proprioceptive sensitivity requires a learning period to regain optimal postural control. It is therefore essential during surgery to respect this new balance as much as possible and to be as minimally invasive as possible. The literature allowed us to identify the sensitive areas in red in the diagram below.
Taking part of the patellar ligament for our reconstruction seemed dangerous to us given the proximity to the sensitive areas with the pressure of the prosthesis, particularly at the level of the kneecap.
We therefore chose a graft with the quadriceps tendon with a suprapatellar incision of less than 5 cm. The residual scar is therefore not an area sensitive to the pressure of the prosthesis and ensures that the patient's sprinting abilities are not weakened.
References: N. Fraisse, N. Martinet, T.-J. Kpadonou, J. Paysant, A. Blum, J.-M. André, Les muscles de l’amputé tibial
https://www.physiostudent.fr/cours/themes/amputation-du-membre-inferieur-1/emboiture-de-la-prothese-15
Installation
- Hanging leg installation with a popliteal support placed under the tibia allows hyperflexion intraoperative
- We also used lateral support
- The intervention was carried out with a pneumatic tourniquet



Surgical technique
For the tibial tunnel, we used an outside-in guide. We incised medially to the anterior tibial tuberosity by making the incision facing the aiming barrel, as small as possible because the area is close to the areas sensitive to the pressure of the prosthesis.
For the femoral tunnel, an outside-in guide was also used with the incision facing the sighting barrel, as small as possible.
The graft was fixed to the femur using an endbutton as well as a biocomposite screw and fixed at the level of the tibia with a biocomposite screw. No meniscal lesion was found during arthroscopic exploration.