Discover the case of a 25 year old recreational athlete who suffered recurrent patellar dislocation and underwent a MPFL reconstruction with harmstring.
The goal of this clinical case is to discuss the therapeutic options in case of persistent patellofemoral instability after MPFL reconstruction.
- 25 Y.O. male
- Recreational athlete, football player
- More than 20 episodes of patellar dislocation
- MPFL reconstruction with hamstring 8 months ago
- Persistent patellofemoral instability, no return to activity due to persistent apprehension
- On physical examination, he presents a 5º extension lag, a positive patellar apprehension and J sign, negative quadrant test and a negative patellar tilt
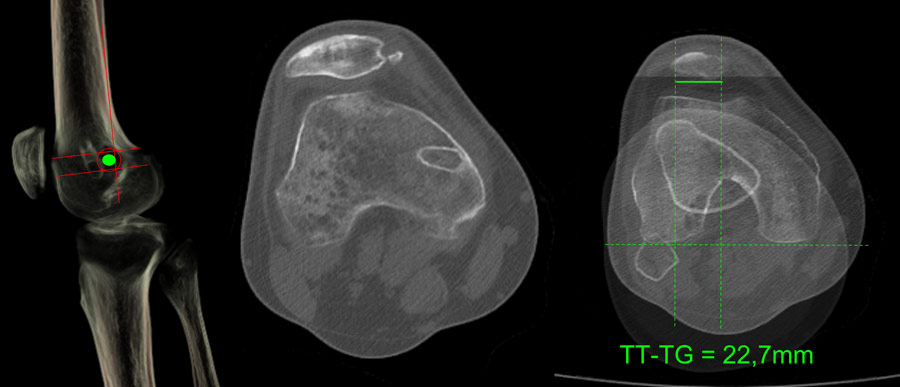
CT
How would you classify this ACL tear?
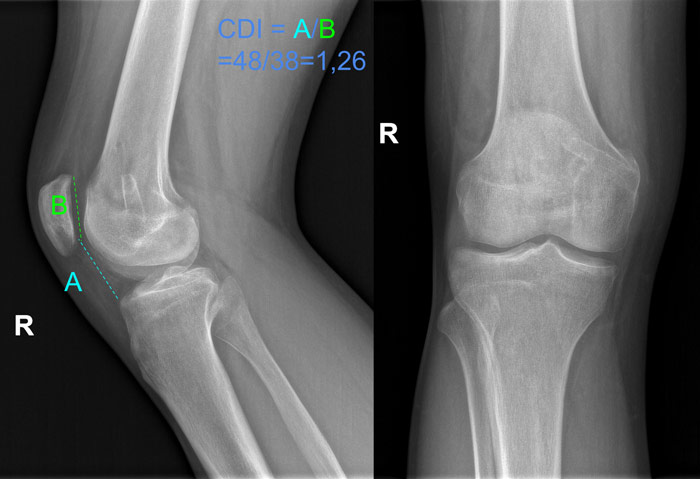
- ✔️Dysplasia type D
According to the Dejour classification of trochlear dysplasia, on a lateral view x-ray of the knee we can identify the “crossing sign” - deepest point of the trochlear sulcus crossing the anterior border of the femoral condyles, the “supratrochlear spur” - a prominent trochlea on the anterior femoral cortex, and the “double contour” - a hypoplastic medial facet of the trochlea.
Kazley JM, Banerjee S. Classifications in Brief: The Dejour Classification of Trochlear Dysplasia. Clin Orthop Relat Res. 2019 Oct;477(10):2380-2386. doi: 10.1097/CORR.0000000000000886. PMID: 31393338; PMCID: PMC6999944.
Which is the cause of the persistent patellar instability?
- ✔️Patella alta
- ✔️Trochlear dysplasia
- ✔️Increased TT-TG distance
A patella alta and a trochlear dysplasia are considered major risk factors that are able to individually lead to patellar dislocation.
David H. Dejour, Guillaume Mesnard, Edoardo Giovannetti de Sanctis Updated treatment guidelines for patellar instability: “un menu à la carte”. Journal of Experimental Orthopaedics 2021 Nov 26;8:109. doi: 10.1186/s40634-021-00430-2. PMCID: PMC8626553 PMID: 34837157
Phillips CL, Silver DAT, Schranz PJ, Mandalia V. The measurement of patellar height. J Bone Joint Surg Br. 2010;92-B(8):1045-1053. doi:10.1302/0301-620X.92B8.23794.
How would you manage this condition?
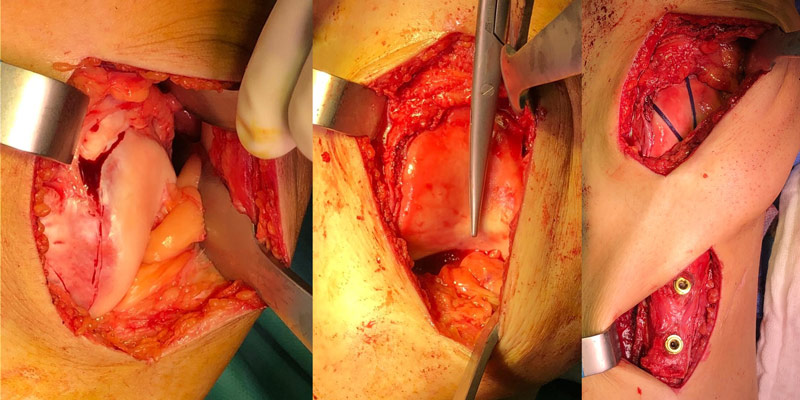
- ✔️Trochleoplasty + tibial tuberosity medialization and distalization + lateral release
In this case, my choice was to keep the original MPFL revision as the patient didn’t have any more patellar dislocation episodes since the index surgery and the MPFL reconstruction seemed competent even though its femoral anchor point is not anatomical, perform a sulcus deepening trochleoplasty as recommended for the treatment of type D trochlear dysplasia and a tibial tuberosity medialization and distalization in order to correct the patella alta and still large TT-TG distance after trochleoplasty was performed This technique complies with the “menu à la carte” guide proposed by Dr. Dejour.
David H. Dejour, Guillaume Mesnard, Edoardo Giovannetti de Sanctis Updated treatment guidelines for patellar instability: “un menu à la carte”. Journal of Experimental Orthopaedics 2021 Nov 26;8:109. doi: 10.1186/s40634-021-00430-2. PMCID: PMC8626553 PMID: 34837157
Dejour, D., Byn, P. & Ntagiopoulos, P.G. The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. International Orthopaedics (SICOT) 37, 433–439 (2013).
Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J Trochleoplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthopaedica 76(5):693–698 (2005).


The immediate and 6 weeks postoperative outcomes are very positive, the patient has control and confidence in his knee. He has a full range of motion and a fully activated extensor apparatus, no pain or apprehension and plans to return to sports.

